by Jim West (please share and cite)
I have strong 'anecdotal evidence' to support these findings. 10 years ago my dentist replaced my mercury fillings with resin though as I belatedly found out when after years he bragged about his use of fluoride to force dental fibers to stand out, to bond better with his resin fillings.
After my initial work by this dentist, I immediately had a ghastly breath odor that could 'kill'. I noticed this unique odor in other people also, on the subway, in NYC where I live. I didn't understand what was happening and was falsely trusting my dentist.
Luckily, with fear, I still refused to obey my dentist's ongoing demands (that I could die of neurological disease associated with gum "infection"). He demanded that I have deep root planing to clean this complex enviro-dentist-made 'infection'.
I was looking for the environmental cause.
Slowly over the years, my gums are recovering since I asked that dentist to halt that procedure. He claimed he had no such knowledge of hazards, but that he would review, and we fell out. His office has a large building extension to handle related surgery etc.
A good dentist/chemist, Gerald Judd (deceased) wrote about this issue with fluoride and periodontal disease. He also warned against root planing, as planing undermines the natural tooth/gum adhesion process and leads to the routine of surgery addiction.
There is a dilemma -- to have cleaning or not when gum complications already exist due to fluoride.
Judd, as a chemist/dentist advised against lemons and vinegar, which can destroy teeth enamel, due to high acidity. I believe that a hazard also exists due to the character of those acids even when diluted, e.g., lemonade. I learned this over the decades the hard way. Phosphoric acid in soda pop has long been known to be a dental hazard. An "iso" version of phosphoric acid in soda pop caused the largest epidemic of paralysis in the history of the USA in the 1930s ("Jake's Leg Syndrome"). That was largest admitted epidemic.
It appears that the entire mercury replacement routine has been scammed into a toxic fluoride delivery mechanism that requires additional dental "treatments" and could lead to dementia etc.
Thankfully, some dentists avoid fluoride and mercury. I presently do not know of any, however, I did find an organization of natural ethical dentists years ago, and may try to dig up the contact info later.
CDC and nGram timelines
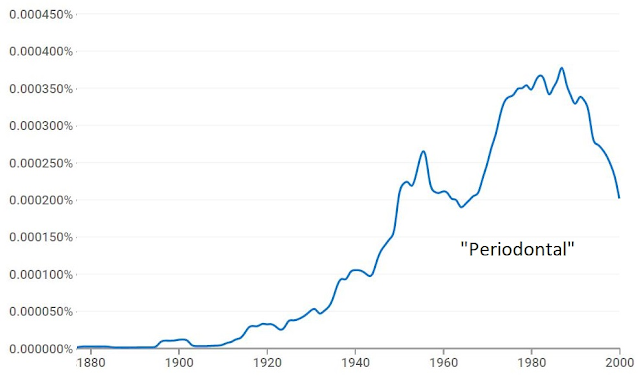
The CDC defends fluoride (of course) however, its timeline matches the usage incidence (Google nGram) of the word "periodontal":
The reason the word usage goes down during 1990s is probably only due to regulated censorship of the word. I doubt incidence is decreasing.
Recent dental consultation
I recently spoke to a dentist about fluoride causation of periodontal disease. I was calm and well prepared.
As if he didn't hear me, he advocated fluoride treatments for periodontal disease.
I was paying for a consultation visit. It lasted 10 minutes with the dentist yelling at me, "Hey man... I'm not trying to poison you!" He was apparently trying to divert attention away from the topic because his assistants were listening. He was speaking the truth though. He need not "try to poison me", because the nature of his work consists of mandated, known and hidden poisonous procedures, beginning with the required X-ray, or as told me, CT-Scan and MRI.
Oblivion...
I additionally mentioned ultrasound cleaning as a hazard, as even AIUM describes an epidemic of carpal tunnel type disease among prenatal ultrasound operators.
He had told me that he had to "let go" of several assistants due to carpal tunnel, which he assumed was due to repetitive use of the computer mouse. I told him that carpal tunnel came about first with the advent of the electric typewriter, but it was as if he could not hear me.
As I paid for my 10-minute consultation at the front desk, I noticed the assistant at the front desk wearing an athletic bandage on her right wrist. Surreal. No one suspected ultrasound nor EMF. As I walked out, I felt as if I was leaving a bizarre carnival house or a house of the insane. My medical views are becoming quite clear, and this was a rare visit to the Medical mainstream.
The following is a fine research article on fluoride, but it does not mention dentist-applied high-concentration fluoride.
From Fluoride Free Water Ireland
Fluoride Exposure: A Major Risk Factor in Periodontal Disease which contributes to Progression of Diabetes, Cardiovascular Disease and Risk of Premature Birth
by Declan Waugh, Environmental Scientist
Summary
Oral disease such as periodontal disease and tooth loss are major public health problems. Untreated, severe periodontal disease is a potential risk for general health and well-being. Periodontal disease results in gum disease, destruction of the alveolar bone and tooth loss. It has also been implicated as a contributing factor in the progression of diabetes, some cardiovascular diseases and the risk of premature birth.[1] The prevalence of periodontal disease is reported to be between 20 and 50% of the worldwide population.[2] Advanced periodontal disease affects up to 15% of the adult population while mild to moderate periodontitis affects most adolescents and 40 to 50% of adults. Between 1993 and 2003 an increase in the proportion of children affected by periodontal disease was observed among 5, 8 and 12 year olds.[3] Among 15 year olds, 56% of 15 year old boys had some periodontal disease distinguishable as gingivitis (inflammation and bleeding of the gums), compared to 48% of girls.[4] The reason for the increased prevalence in recent years is not fully understood.
Many studies and published documents have demonstrated that increased fluoride exposure is directly linked to increased periodontal disease. From a public health perspective, any study that demonstrates increased fluoride exposure may increase the risk of developing periodontal disease or other illnesses are of major importance. This is especially the case when Ireland has globally one of the highest prevalences of periodontal disease combined with the highest number of premature deaths from ischemic heart disease in the EU[5] and periodontal disease is associated with increased risk of cardiovascular disease.
The Irish Expert Body on Fluoride and Health have claimed that “there is no credible evidence linking fluoride and periodontal disease”[6]. This paper examines the available evidence and shows that there appears to be credible scientific evidence to support this relationship. These findings highlight the need for urgent review of public health policy regarding fluoridation of drinking water supplies in Ireland.
1. Introduction
This paper will attempt to highlight some of the available research supporting the relationship between fluoride exposure and increased risk of periodontal disease. It further aims to address the lack of available evidence noted by the Irish Expert body on this subject area. It provides a history of published studies by reputable professionals in peer-reviewed journals as well as medical and scientific evidence from other published sources. The review demonstrates that credible evidence in the field of oral health exists linking fluoride exposure to periodontal disease. Ireland is the only country in the EU with a mandatory policy of artificial fluoridation of public drinking water supplies thereby resulting in increased dietary fluoride exposure of the population compared to other EU Member states.
Despite the Irish Expert Body on Fluoride and Health and Dental Health Foundation Ireland claiming that water fluoridation is the most effective method in the prevention and treatment of dental decay, after over four decades of mass fluoridation of Irish citizens, Ireland has one of the highest prevalences of Edentulous (tooth loss) in EUGLOREH countries. Similarly there has been little improvement in dental health in children especially compared to every other European country where in the same timeframe enormous improvements have occurred (without the need for fluoridation of drinking water) resulting in overall better dental health. Considering that evidence from countries such as Chile, Japan, Finland, the Netherlands and Germany clearly demonstrates that upon cessation of water fluoridation dental health improved significantly within the population, it is entirely possible that reduced fluoride exposure may have had a beneficial impact on dental health.
In comparison, the dietary exposure of the Irish population to fluoride compounds is expected to be much higher due to a long-term exposure of the population to fluoridated water using silicofluoride chemicals, the widespread use of fluoridated toothpastes as well as a much greater consumption of tea and higher overall usage of prescribed drugs, many of which are fluoride-based pharmaceuticals. According to the European Food Safety Authority each of these may be significant contributory sources of fluoride. It is to be expected therefore that the Irish population will have a much greater exposure to fluoride compared to other European countries.
The results of a recent EU wide study[7] supported this observation where children in Ireland were recorded to have, within the EU study region, the highest concentration of fluoride in their urine as well as the highest prevalence of dental fluorosis. Any evidence of association between higher fluoride intake and disease prevalence is therefore of enormous public health importance.
2. Historical evidence
In 1936 Dean H.T. D.D.S- wrote in the Journal of the American Medical Association:
"From observations that I made in areas of relatively high fluoride concentration (more than 4 parts per million of fluorine) there is sufficient evidence to suggest that there is an apparent tendency toward a higher incidence of gingivitis (periodontal disease) ."[8]
Similar observations of the link between fluoride and periodontal disease have been made many times since by Dean & Arnold, 1943[9]; Day, 1940[10]; Spira L. 1953[11]; Ramseyer et al, 1957[12]; Grimbergen et al, 1974[13]; Poulsen & Moller,1974[14]; Waldbott et al, 1978[15]; Olsson, 1979[16]; Reddy et al, 1985[17]; Wei et al, 1986[18] and Yiamouyiannis, 1993[19].
In 1953, Leo Spira had identified gingivitis and bleeding gums as signs of chronic fluoride poisoning. In 1956 the link between fluoride exposure and periodontal disease was further established. Dr. Charles Dillon documented that fluoride causes a progressive degeneration of vital tissue in the root and the dental periosteum, the membrane which separates the tooth from the bone.[20] This results in the progressive periodontal (gum) disease and in wholesale loss of teeth. The action of fluoride on teeth Dr. Dillon demonstrated is not the same in everyone residing in fluoridated areas. There are wide variances depending on geology of the area where people live, a person constitutional and nutritional state are all factors that act to influence the extent of damage fluoride may do to teeth. [21] Prior to this the American Journal of Public Health published an article[22] by Dr. M.C. Smith and Dr. H.V. Smith entitled “Observations on the Durability of Mottled teeth” found that Dental fluorosis or mottled teeth resulting from overexposure to fluoride are structurally weak, and when decay does set in, the result may often be disastrous resulting in the tooth cracking inability to repair the teeth and ultimately resulting in extraction.
In 1952 Dr. V.O. Hurme, D.M.D., former Director of the famous Forsythe Dental Infirmary for children in Boston stated[23]
“Among the very inadequate studies, physical signs of fluoride toxicosis are inflammation and destruction of the gingival and periodontal (gum tissue). Published and unpublished observations by many men suggest rather strongly that periodontoclasia (gum disease) may be induced or aggravated by certain chemicals, including fluoride.”
This conspicuous evidence of fluoride poisoning, Dr. Hurme cautioned, may not always show up as a warning sign. He stated:
“Once enamel formation is completed the intake of fluoride has little or not visible effect on normal enamel. Thus it follows that when the crowns of the third molars are fully calcified, the visible parts of the teeth cease to serve as indicators or excessive fluoride intake.”[24]
In 1957, Ramseyer observed gingivitis in older rats drinking water fluoridated at 1 ppm. While in 1972 Domazalska observed a direct correlation between the severity of periodontal disease in humans and fluoride levels in systemic fluids.[25]
3. Recent literature
Research documentation from the pharmaceutical company Sepracor[26] (renamed Sunovion Pharmaceuticals Inc), indicates that fluoridated toothpaste may cause or contribute to periodontal bone loss. This finding is serious because periodontal bone loss is the number one cause of tooth loss among adults. Patents supplied by the pharmaceutical company disclosed that concentrations of fluorides from fluoridated toothpastes and mouthwashes activate G proteins in the oral cavity, thereby promoting gingivitis and periodontitis, as well as oral cancer. The patent findings supply the biochemical explanation for earlier reports by many researchers who had found increased gingivitis and gum inflammation due to fluoridated water, or other sources of fluoride. In 1996 three biochemists Aberg G, Jerussi TP and McCullough JR working for Sepracor investigated fluoride implications in periodontal disease. Realizing that fluorides activate G proteins, they reasoned that fluorides would also be involved in the activation of those G proteins which regulate the pathways involved in gingivitis and periodontitis - and they decided to test for the ability of fluoride to activate two integral receptors involved in periodontal disease - the prostaglandin E2 receptor (PGE2) and the thromboxane A2 (TXA2) receptor. Both are coupled to G proteins called G q/11. The scientists conducted a test with sodium fluoride based on a well-established in-vitro protocol model involving HL-60 cells. These are Human Leukemia cells often used in biochemistry investigations, as one can observe fundamental and critical signals involved in the activation of the body's immune system - because of the cells’ ability to respond to foreign organisms. The authors reported:
"We found that fluoride, in the concentration range in which it is used for the prevention of dental caries, stimulates production of prostaglandins and thereby exacerbates the inflammatory response in gingivitis and periodontitis.... Thus, the inclusion of fluoride in toothpastes and mouthwashes for the purpose of inhibiting the development of caries may, at the same time, accelerate the process of chronic, destructive periodontitis."
However, instead of alerting the public health officials to their findings, they went looking for an agent which would counteract the adverse effects of fluoride choosing a non-steroidal anti-inflammatory agent (NSAID) called ketoprofen. They conducted more studies[27] to see if ketoprofen was efficient in offsetting the damaging fluoride affects, and in 1996 filed a patent on their new concoction now containing both fluoride and ketoprofen. In 1998 they obtained a patent[28] for a topically applied fluoride product in which they state that:
“The present invention is a method for preventing dental caries by administering a fluoride salt into the oral cavity while at the same time controlling periodontal bone loss by administering, in addition to the fluoride salt, an amount of an NSAID sufficient to inhibit the production of prostaglandins induced by the fluoride.”
The patent findings implicating the fluoride "topical" activation of G proteins in the oral cavity have many far-reaching and serious implications - not only for periodontal disease, but also for oral cancers - which involve "mutated" G proteins, and which are activated by fluoride, often even "preferring" fluoride activation. Subsequently, a study was instigated at the Harvard School of Dental Medicine (funded by Sepracor), documenting the beneficial effects of ketoprofen upon gingivitis. The first study on beagles included one of the three co-inventors (McCullough) together with two Assistant Professors from two separate well-respected Universities, and was subsequently published[29] in the Journal of Clinical Periodontology in 1997. The study concluded:
“Systemic and topical administration of non-steroidal anti-inflammatory drugs (NSAIDs) has been shown to reduce periodontal disease progression in both animal models and human subjects.”
Curiously despite the authors known previous findings regarding this drug no mention was made of fluoride in the study. (Ref: PFPC Newsletter 9 http://www.whale.to/a/pfpc_newsletter_9.html)
According to Lee J et al.[30] Sodium fluoride (NaF) has been shown to be cytotoxic and produces inflammatory responses in humans. Gingivitis and periodontitis account for more than 95% of all inflammatory diseases of the tissues surrounding the teeth.[31] Lee’s results suggest that NaF induces apoptosis (programmed cell death) in human gingival fibroblasts (HGF) through both the mitochondria-mediated pathways regulated by the Bcl-2 family and death receptor-mediated pathway and may play a role in the development of periodontal disease.
Dr. Ken Yaegaki and co-workers at the Nippon Dental University, Tokyo, reported[32] finding significant increases in a dose dependent manner of apoptosis or necrosis/late apoptosis of human gingival epithelial cells exposed in cultures to NaF they cite evidence that the regular use of fluoridated toothpastes and mouth-rinses might involve periodontal soft tissue F sensitivity in subjects of different ages.
Given that apoptosis of gingival crevicular epithelial cells has been shown to be one cause of periodontal pathology[33] gingivitis could conceivably be a response to F effects. Further studies have demonstrated that F at higher concentrations than in saliva might involve periodontal pathologic changes, since F sensitivity is different within different cells or different ages of the subjects,[34],[35] and as very low concentration of NaF (5 mg/L) caused apoptosis in osteoblasts, which also play an important role in periodontal pathology.[36]
These observations are comparable to the results obtained by Jeng et al.[37] when they reported that increasing concentrations of fluoride showed cytotoxicity to human oral mucosal fibroblasts.
There is a long history of association between the critical role of smoking on the incidence and severity of periodontal disease.[38],[39] It is now generally accepted that cigarette smoking is a significant risk factor for periodontal disease.[40] In 1983, Ismail et al.[41] analyzed smoking and periodontal disease and found that after adjusting for potential confounding variables such as age, oral hygiene, gender and socioeconomic status, smoking remained a major risk indicator for periodontal diseases. Locker and Leake[42] found that among Canadians, smoking was one of the most consistent predictors of periodontal disease experience. Two similar population-based epidemiologic studies have found that periodontitis is more common in smokers than nonsmokers [43],[44] and it has also been reported that smoking is associated with an increase in serum inorganic fluoride concentration.[45] It is likely that the fluoride content of tobacco is the single most significant risk factor in this association.
Similarly a recent study Simpson et al.[46] on the bioavailability of fluoride (from tea) demonstrated that fluoride was retained in the oral cavity where it shows a strong binding ability to interact with the oral tissues and their surface integuments. This is to be expected as Yadav AK et al.[47] reported that tea, toothpaste, tobacco, and dental mouthwashes (with tobacco and without tobacco use) are significant sources of total dietary fluoride intake demonstrating that they frequently expose the human body to 3.88-137.09, 53.5-338.5, 28.0-113.0, 16.5-306.5 and 23.5-185.0 microg of fluoride per gram of these items, respectively. Fluoridation of drinking water and its subsequent contribution of fluoride compounds to other food products through processing and cooking with fluoridated water would increase dietary fluoride exposure further. It is plausible to suggest therefore that total dietary intake of fluoride may be a major risk factor to the development of periodontal disease.
A link between Osteoporosis and periodontal disease was also reported in the British Medical Journal by Dr. John Coventry, Professor of Periodontology at University of London in 2000.[48] It is widely accepted that osteoporosis is associated with fluoride exposure. The European food safety authority have established for adults an upper tolerable limit for fluoride based on a risk of bone fracture.[49] Fractures are the most dangerous aspect of osteoporosis.
In 2002, the U.S Centers for Disease Control published a report on Public health and Aging examining the retention of natural teeth amongst adults.[50] While the report noted that during the past several decades, the percentage of older adults who have retained their natural teeth has increased steadily the findings of the report raised some significant questions. Hawaii and California had the lowest rates of water fluoridation in the USA: 8.8% of the population in the state of Hawaii was fluoridated; 27.7% of the population in the state California was fluoridated. Kentucky had the highest rate of water fluoridation with virtually 100% (99.7%) of the population receiving fluoridated drinking water. In 2003, the American Dental Association awarded Kentucky with a “50 Year Award” for virtually 100% fluoridation for 50 years.[51]
The CDC as with the Health Department in Ireland have claimed that community water fluoridation is the most effective method for preserving oral health. If tooth loss is a measurement of oral tooth health, then one would expect to see much lower rates of edentulism (tooth loss) in fluoridated communities. This has not occurred in the U.S nor coincidentally has it occurred in Europe (Fig 1) where much higher rates of tooth loss are also reported in fluoridated communities.
Generally speaking, it is apparent that when the percentage of fluoridated individuals increases, so does the percentage of people with missing teeth. There appears to be no life long reduction in dental decay that can be directly attributable to water fluoridation and instead there appears to be an increase in tooth loss associated with fluoridation amongst the older population who have the longest exposure compared to non fluoridated communities.
The CDC report findings would support this in noting:
“The prevalence of edentate persons (i.e., those who have lost all their natural teeth) ranged from 13% in Hawaii and California to 42% in Kentucky.”
The lowest rates of tooth loss in people over 60 years of age occur in the states with the lowest rates of water fluoridation.
While in Europe the prevalence ranged form 48% in fluoridated Republic of Ireland to 17% in Sweden, 18% in Denmark, 15 % in Italy, 36% in the UK and 40% in Northern Ireland. In other words, the highest rates of tooth loss in people over 60 years of age occur in the regions with the highest rates of water fluoridation.
It is likely that the higher incidence of dental fluorosis recorded in fluoridated communities, itself a visible sign of overexposure to fluoride, is also a contributor to this phenomenon. However it should be noted, that this in itself is not an accurate reflection of fluoride exposure generally in the population, as the teeth of children over 8 years of age will not develop dental fluorosis regardless of fluoride dietary exposure.
In 2007 researchers reported this link between dental fluorosis and periodontal disease in the Indian Journal of Dental Research. [52] also reported in the British Dental Journal.[53] It was observed that increased fluoride exposure resulted in increased periodontal disease. The study concluded:
“The results suggest that there is a strong association of occurrence of periodontal disease in high-fluoride areas. The role of plaque is well understood in contrast to the effect of fluorides on periodontal tissues. Fluoride must therefore be considered an important etiological agent in periodontal disease.”
This was further examined in 2011 when a study by Lutfioglu et al.[54] evaluating the influence of fluoride on periodontal soft tissues demonstrated that excessive fluoride consumption may alter the periodontal tissue homeostasis which may be detrimental in the maintenance of periodontal health.
A further study in 2011 published in the Indian Journal of Dental Research[55] concluded that,
“the association between degree of fluorosis and periodontal status is statistically significant.”
4. Conclusion
Based on these facts, fluoridation does not appear to have helped prevent tooth loss and clearly it is evident that fluoridation does not benefit those without teeth. What is known is that during the last 80 years a clear association between periodontal disease and fluoride exposure was identified and reported, however considering the significance of the disease it is also apparent that it was not studied in the detail one would expect. The bulk of the research has been on dental caries not periodontal disease.
It is clear however that evidence demonstrating a link between total dietary fluoride exposure and periodontal disease is available if you look for it. It is further evident that based on the current information available and on the understanding of the ‘precautionary principle’ that a cessation of the policy of mandatory fluoridation of public drinking water supplies should be undertaken immediately to assist in reducing the exposure of the population to fluoride to acceptable safe levels. One cannot control the dietary exposure to fluoride compounds for all sectors of the population by fluoridation of public water supplies. It is certain for large sectors of the population that fluoridation of water supplies only increases the risk of potential harm.
References
[1] European Commission, Health in Europe, Dental and Oral Diseases.
[2] European workshop in periodontal health and cardiovascular disease—scientific evidence on the association between periodontal and cardiovascular diseases: a review of the literature, Eur Heart J Suppl (2010) 12 (suppl B): B3-B12.
[3] European Commission, Health in Europe, Dental and Oral Diseases.
[4] World Health Organization (WHO). Resolution WHA60.17 Oral health: action plan for promotion and integrated disease prevention. WHO, Geneva, Switzerland. (2007)
[5] HSE Cardiovascular Health 2010.
[6] Review of Waugh Report on Human Toxicity, Environmental Impact and Legal Implications of Water Fluoridation. Dr Joe Mullen, Irish Expert Body on Fluorides and Health, May 2012
[7] EU Biomed Flint Project
[8] H. TRENDLEY DEAN, D.D.S. Chronic Endemic Dental Fluorosis (Mottled Enamel), JAMA. 1936;107(16):1269-1273.
[9] Dean, H.T.; Arnold, F.A., Jr.; and Elvove, E. (1942): Domestic Water and Dental Caries. V. Additional Studies of the Relation of Fluoride Domestic Waters to Dental Caries Experience in 4,425 White Children, Aged 12 to 14 Years, of 13 Cities in 4 States, Pub Health Rep 57:1155-1179.
[10] Day, M.: Chronic Endemic Fluorosis in Northern India. Br. Dent. J., 68:409-424, 1940.
[11] Spira L, MD, Ph.D. "The Drama of Fluorine -Arch Enemy of Mankind" Milwaukee, Wisconsin: Lee Foundation, 1953
[12] Ramseyer WF, et al. (1957). Effect of Sodium Fluoride Administration on Body Changes in Old Rats. J Gerontol. 12: 14-19.
[13] Grimbergen G. A double blind test for determination of intolerance to fluoridated water (preliminary report). Fluoride 7:146-152. (1974).
[14] Poulsen, S. and Moller, LJ.: Gingivitis and Dental Plaque in Relation to Dental Fluorosis in Man In Morocco. Arch. Oral. Biol., 19:951-954, 1974
[15] Waldbott GL, Lee JR. 1978. Toxicity from repeated low grade exposure to hydrogen fluoride. Case study Clinical Toxicology 13:391-402
[16] Olsson B.1978 Dental findings in High Fluoride Areas In Ethopia. Community Dentistry and oral epidemiology, 7,51-56
[17] Reddy, J, Grobler SR, Reiter NF. 1988. The relationship of the periodontal status to fluoride levels of alveolar bone and tooth roots. Journal Clinical Periodontol 15:217-221
[18] Wei SJY, Yang S, Barmes DE. Needs and implementation of preventive dentistry in China. Community Dent Oral Epidemiol 1986;14:19-23.
[19] Yiamouyiannis JA. Fluoridation and cancer: The biology and epidemiology of bone and oral cancer related to fluoridation. Fluoride 1993;26(2):83-96.
[20] Dillon, Chas.: The significance of Fluoridation Statistics, Dental Digest 62:362 (1956)
[21] George L. Waldbott M.D. A struggle with Titans, Carlton Press 1965
[22] Smith, M.C and Smith, H.V.: ““Observations on the Durability of Mottled teeth” Dental Mottled teeth identifiable as dental fluorosis. American Journal of Public Health 30:1050 (1940).
[23] Hurme, V.O: “An examination of the Scientific Basis for Fluoridating Populations,” Dental Items of Interest, (June 1952)
[24] George L. Waldbott M.D. A struggle with Titans, Carlton Press 1965
[25]W. Domazalska, Incidence of periodontal diseases in subjects with various degree of exposure to fluorides, Czas Somatol 25 (1972), p. 1005.
[26] Sepracor Inc. is a U.S. research-based pharmaceutical company involved in researching, developing and commercializing innovative pharmaceutical products. In October 2009, Sepracor Inc. was acquired by Dainippon Sumitomo Pharma Co., Ltd. (DSP), a top ten, stock exchange-listed pharmaceutical company based in Osaka, Japan.
[27] Aberg G, Ciofalo VB, Pendleton RG, et al. Inversion of (R)- to (S)-ketoprofen in eight animal species. Chirality 1995; 7(5): 383-7
[28] NSAID/fluoride periodontal compositions and methods" US Patent: 5,807,541, granted September 15, 1998.
[29] D.W. Paquette et al. Enantiospecific inhibition of ligature-induced periodontitis in beagles with topical (S)-ketoprofen, Journal of Clinical Periodontology, Volume 24, Issue 8, pages 521–528, August 1997.
[30] Lee J et al. Involvement of both mitochondrial- and death receptor-dependent apoptotic pathways regulated by Bcl-2 family in sodium fluoride-induced apoptosis of the human gingival fibroblasts, Toxicology Volume 243, Issue 3, 20 January 2008, Pages 340–347
[31] Roy C. Page, DDS, PhD; L. David Engel, DDS, PhD; A. Sampath Narayanan, PhD; James A. Clagett, PhD, Chronic Inflammatory Gingival and Periodontal Disease, JAMA. 1978;240(6):545-550.
[32] Herai, Yaegaki, Murata, Sato, Imai, Tanaka, Itai, Induction Of Apoptosis In Human Gingival Epithelial Cells By Sodium Fluoride, Fluoride 42(1)3–8, January-March 2009
[33] Ekuni D, Tomofuji T, Yamanaka R, Tachibana K, Yamamoto T, Watanabe T. Initial apical migration of junctional epithelium in rats following application of lipopolysaccharide and proteases. J Periodontol 2005;76:43–8.
[34] Sato T, Yagori A, Niwa M. Low sensitivity of cultured human young adult and adult gingival fibroblasts to fluoride. I. Relation to doubling time. Pharmacol Toxicol 1987;61:313–5
[35] Hongslo CF, Hongslo JK, Holland RI. Fluoride sensitivity of cells from different organs. Acta Pharmacol Toxicol 1980;46:73–7.
[36] Yan X, Feng C, Chen Q, Li W, Wang H, Lv L, et al. Effects of sodium fluoride treatment in vitro on cell proliferation, apoptosis and caspase-3 and caspase-9 mRNA expression by neonatal rat osteoblasts. Arch Toxicol 2008 Oct 21. [Epub ahead of print].
[37] Jeng JH, Hsieh CC, Lan WH, Chang MC, Lin SK, Hahn LJ, et al. Cytotoxicity of sodium fluoride on human oral mucosal fibroblasts and its mechanisms. Cell Biol Toxicol 1998;14:383–9.
[38] Ana Pejčić Et Al. Smoking And Periodontal Disease A Review, Medicine And Biology Vol.14, No 2, 2007, Pp. 53 - 59
[39] Erdemir EO, Duran I, Haliloglu S. Effects of smoking on clinical parameters and the gingival crevicular fluid levels of IL-6 and TNF-α in patients with chronic periodontitis. J Clin Perio 2004; 31: 99-104.
[40] Deborah M. Winn, Tobacco Use and Oral Disease Journal of Dental Education ■ Volume 65, No. 4
[41] Ismail AI, Burt BA, Eklund SA. Epidemiologic patterns of smoking and periodontal disease in the the United States. JADA 1983; 106: 617-623.
[42] Locker D, Leake JL. Risk indicators and risk markers for periodontal disease experience for older adults living independently in Ontario, Canada. J Dent Res 1993; 72: 9-17.
[43] Beck JD, Koch GG, Rozier RG, Tudor GE. Prevalence and risk indicators for periodontal attachment loss in a population of older community-dwelling blacks and whites. J Periodontol 1990;61:521-8.
[44] Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol 2000;71:743-51
[45] M. Laisalmi ey al. Fluoride metabolism in smokers and non‐smokers following enflurane anaesthesia Br. J. Anaesth. (2003) 91 (6): 800-804.doi: 10.1093/bja/aeg272
[46] Simpson A, Shaw L, Smith AJ. The bio-availability of fluoride from black tea. J Dent. 2001 Jan;29(1):15-21.
[47] Yadav AK, Kaushik CP, Haritash AK, Singh B, Raghuvanshi SP, Kansal A. Determination of exposure and probable ingestion of fluoride through tea, toothpaste, tobacco and pan masala. J Hazard Mater. 2007 Apr 2;142(1-2):77-80. Epub 2006 Jul 29.
[48] Coventry et al. Clinical Review ABC of oral health Periodontal disease BMJ 2000;321:36
[49] EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (EFSA 2005)
[50] Public Health and Aging: Retention of Natural Teeth Among Older Adults United States, 2002, Centres for Disease Control.
[51] (http://www.skagitcleanwater.com/Fluoridatio_concern_%20Brief_%200utline.pdf)
[52] Vandana KL, Reddy MS. 2007 Assessment of Periodontal Status in Dental Fluorosis Subjects using Community Periodontal Index of Treatment Needs. Indian Journal of Dental Research 18(2):67-71.
[53] Fluoride linked to gum disease, News British Dental Journal 202, 647 (2007) Published online: 9 June 2007 | doi:10.1038/bdj.2007.503
[54] Lutfioglu M. et al. Excessıve fluorıde ıntake alters the MMP-2, TIMP-1 and TGF-β levels of perıodontal soft tıssues: an experımental study ın rabbıts. Clin Oral Invest (2012) 16:1563–1570
[55] Kumar, PR, John J. Assessment of periodontal status among dental fluorosis subjects using community periodontal index of treatment needs. Indian J Dent Res. 2011 Mar-Apr; 22(2):248-51.
____________________________________________




Mr. West, I'm thoroughly grateful I found your work (from reading Jon Rappoport's blog). Another wildly informative article. Your sagacity and insight deserves a wider audience, however I understand the reality of the world we live in, even within the 'truth/medical freedom' communities. Please keep up the great work.
ReplyDeleteThanks!
DeleteWhat do you think of Dr. Bryan Ardis "venom in the water" theory ?
ReplyDeleteThat theory is related to COVID, a respiratory disease. Air pollution makes more sense.
ReplyDeletehttps://harvoa-med.blogspot.com/2020/04/COVID2020.html?m=1